
The retina is a thin layer of tissue in the back of the eye that senses light and allows us to see. Unfortunately, this delicate and intricate tissue can be affected by different conditions and diseases. In the United States alone, over 20 million people are affected by retinal disease, and if left untreated, such conditions can lead to blindness.
Our retina specialists, Dr. Brian Phillpotts and Dr. Alfonso Ponce, along with the rest of our retina team, are experienced in treating vitreoretinal diseases, including diabetic retinopathy, macular degeneration, retinal detachment, macular holes, and other vitreoretinal diseases and disorders.
Many questions often surround retinal diseases and other vitreoretinal disorders—click here to read through the most frequently asked questions about retina diseases and answers from our retina specialists.
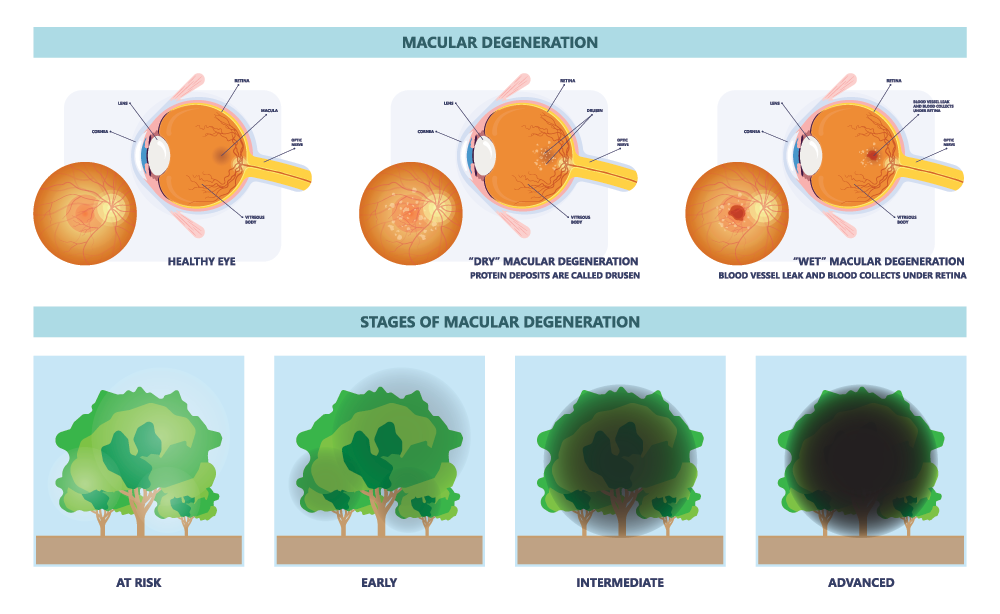
Macular degeneration (AMD) is an age-related degenerative condition of the macula. It is the most common cause of vision loss in the United States in those 50 or older, and its prevalence increases with age. AMD is caused by hardening of the arteries that nourish the retina. This deprives the sensitive retinal tissue of oxygen and nutrients that it needs to function and thrive. As a result, the central vision deteriorates. The macula is the center of the retina that controls sharp, straight-ahead vision; damage to the central retina leads to difficulty reading, seeing fine details, and recognizing faces.
AMD is a condition that develops very slowly in some people and much faster in others, and its prevalence increases with age. Macular degeneration varies widely in severity. In its worst cases, it causes a complete loss of central vision, making reading or driving impossible. For others, it may only cause slight distortion. Fortunately, macular degeneration does not cause total blindness since it does not affect peripheral vision. Some people with AMD may not notice any changes at all.
Dry AMD:
The majority of people with AMD have dry AMD (sometimes called atrophic AMD)—dry AMD makes up about 90% of the cases of AMD. With this type of AMD, the macula thins with age. Those with this type of AMD may have yellow deposits, known as drusen in the macula. A couple of small drusen may not impact one’s vision, but as they get bigger and become more numerous, they can distort or dim vision and lead to central vision loss.
Dry AMD occurs in 3 stages: early, intermediate, and advanced. It typically progresses slowly over several years. There are currently no approved treatments for dry AMD. Still, there are steps one can take, such as consuming specially formulated vitamins, to decrease the risk of the condition progressing into its most advanced form.
Wet AMD:
Wet AMD, also known as neovascular AMD, is a less common and more serious type of advanced AMD—only about 10% of people with macular degeneration have this form. With this type of AMD, abnormal blood vessels grow under the macula and bleed and leak fluid into the retina. This can cause vision to become distorted, create blind spots, and can lead to a loss of central vision. These blood vessels are like weeds growing through cracks, and eventually, they form a scar which can lead to permanent loss of central vision.
Any stage of dry AMD can progress into wet AMD, but wet AMD is always the late stage of this condition. Compared to dry AMD, wet AMD progresses more quickly and can cause patients to experience more significant vision loss. However, if caught early enough, there are treatment options that can stabilize a patient’s vision and lower the risk of experiencing further vision loss.
Anti-VEGF medications are the most widely used treatment for wet AMD. These medicines are injected into the eye to help stop blood vessel growth and bleeding. Certain nutritional supplements have been shown to be beneficial for dry macular degeneration when other treatments are not appropriate.
A retinal detachment occurs when the retina’s sensory and pigment layers separate. The retinal cells may become severely deprived of oxygen, increasing the risk of suffering from permanent vision loss. The longer these cells are separated from the retina, the more likely a person will experience a permanent loss of vision. Retinal detachment is considered an ocular emergency that requires immediate medical attention because it can cause devastating damage to the vision if left untreated. It is a problem that occurs most frequently in the middle-aged and elderly.
Early detection of retina conditions is crucial in successfully treating the problem. Awareness of the quality of your vision in each eye is critical, especially for those at an increased risk due to age or other health concerns.
Rhegmatogenous retinal detachment is the most common type of retinal detachment. This occurs when there is a break in the sensory layer of the retina, and fluid seeps underneath, causing the layers of the retina to separate. Those who are very nearsighted, have undergone eye surgery, or have experienced a serious eye injury are at greater risk for this type of detachment. Nearsighted people are more susceptible to experiencing a rhegmatogenous retinal detachment because their eyes are longer than average from front to back, causing the retina to be thinner and more fragile.
A tractional retinal detachment is the second most common type of retinal detachment. This occurs when strands of vitreous or scar tissue create traction on the retina, causing it to pull away from the back of the eye and detach. Patients with diabetes are most likely to experience this type of retinal detachment. When diabetic retinopathy is inadequately controlled or improperly taken care of, it can lead to issues with the retinal vascular system. This vascular damage can eventually accumulate scar tissue in the eye that could cause retinal detachment.
The third type of retinal detachment is exudative detachment. In cases of exudative detachment, there are no tears or breaks in the retina. Instead, it occurs when fluid collects underneath the layers of the retina, causing the retina to separate from the back wall of the eye. This type usually occurs in conjunction with another disease affecting the eye that causes swelling or bleeding. Retinal diseases such as the following cause this type of detachment:
● An inflammatory disorder that causes fluid to build up behind your retina
● Wet macular degeneration
● Cancer behind your retina
● Coats’ disease, which causes abnormal development in the blood vessels leading to leaking proteins building up behind the retina
There is no pain related to retinal detachment, but there is usually some discomfort and a few symptoms before the retina becomes detached.
Primary symptoms include:
● Blurred vision
● Partial vision loss, which makes it seem as though a veil or curtain has been pulled across your field of vision, giving off a dark, shadowing effect
● Sudden flashes of light that appear in your peripheral vision.
● Suddenly seeing a new shower of floaters, which are tiny pieces of debris that look like black flecks or strings floating before your eye
● An increase in existing flashes and/or floaters
Call Dr. Phillpotts or Dr. Ponce immediately if you begin to experience any of the above symptoms, as retinal detachment requires urgent evaluation and treatment.
Early detection of retina conditions is crucial in successfully treating the problem. Awareness of the quality of your vision in each eye is vital, especially for those at an increased risk due to age or other health concerns.
Notify Dr. Phillpotts or Dr.Ponce immediately if you notice any of the following:
● Sudden loss of vision
● An obstruction of your peripheral vision (a veil, shadow, or curtain)
● Sudden shower of floaters
● Flashes of light
● Distorted vision on an Amsler grid or straight lines of a doorway or edge of a window appearing bent. The appearance of spots, bugs, or spider webs
Request an Appointment with one of St. Luke’s retina specialists today.
We proudly serve patients at our eye clinics in Tarpon Springs, Tampa, St. Petersburg, Clearwater, Spring Hill, Wesley Chapel and in The Villages at Lake Sumter Landing and Brownwood. Our philosophy is to treat those we serve as though they are a member of our own families. From the first phone call or email to the follow-up visit and beyond, we’re here to serve you. Our goal is to help preserve and optimize your vision.